Joint Replacement: Get Back in the Game – Broward Health North

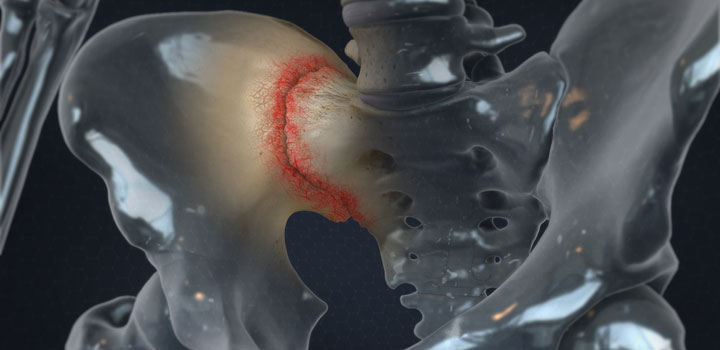
Osteoarthritis is the most common form of arthritis affecting more than 25 million people. It is genetic and causes pain, stiffness and destruction within the joint. Common sites of osteoarthritis include the hip, knee, fingers and shoulders. Some patients develop post-traumatic arthritis, which is arthritis that develops months or years after a major injury or fracture in or around a joint. Other forms of arthritis include rheumatoid arthritis and psoriatic arthritis. These are inflammatory diseases which affect the lining of the joints and often affect multiple joints in the arms and legs.
Osteoarthritis symptoms can be managed by anti-inflammatory medicines such as ibuprofen and naproxen. Physical therapy can help maintain flexibility in the joint and can strengthen the muscles around the arthritic joint. At its most advanced stages, Osteoarthritis causes severe pain and stiffness. Once the pain interferes with your daily activities and is no longer responding to conservative treatment, surgery is the treatment of choice.
A recent patient was suffering from a weak knee for nearly 40 years after developing post traumatic arthritis and stiffness after two initial surgeries when he was in the military. He underwent a successful total knee replacement in 2019 using computer-assisted navigation. He participated in inpatient physical therapy and went home two days after surgery. Seven weeks after surgery, this patient has no pain in his knee, he has much better flexibility and has just returned from a two week hike in the Smokey Mountains. A successful total knee replacement has restored his quality of life.
Total joint replacement (TJR) is one of the most commonly performed, elective surgical procedures in the United States, and the volume of primary and revision TJR procedures has risen continuously in recent decades. According to PubMed.gov, hip replacements are projected to grow 71% by 2030 and total knee replacements are projected to grow 85%, by 2030.
Joint replacement or other surgeries are sometimes considered the “treatment of last resort” for people with osteoarthritis. Doctors frequently tell patients to wait as long as possible before joint replacement, but to get the best results, it should also not be delayed too long. How do you know when it’s time to seek joint replacement surgery?
If you’ve unsuccessfully attempted conservative treatment or if damage to the cartilage or bone is beyond repair, remember that joint replacement is proven to be safe and highly effective in the right patient. Dr. Janke says this is still often your best option. Newer techniques in the hip and knee can give patients excellent pain relief and improved function.
Talk with your doctor about the best options and long-term strategies for you and understand what’s available for your specific problem. Preserving your joints and your activities and lifestyle is the basis for a partnership that is best for you.
If you need an orthopedic surgeon near you, visit BrowardHealth.org/Find-Doctor. To learn more about Broward Health North’s Joint Replacement Center, call 954.712.4274.
https://pubmed.ncbi.nlm.nih.gov/30180053/
https://aaos-annualmeeting-presskit.org/2018/research-news/sloan_tjr/