Osteonecrosis: Treatment
The Concept of Risk/Benefit Ratio
Before entering into a description of some of the treatments available for osteonecrosis, it is important that this concept be understood. Any surgical procedure has a certain element of risk involved. Even no treatment at all has the risk that the disease will progress, so doing nothing is not risk free. Some procedures may have a lower likelihood of success but may have a very little downside risk. Other procedures may have a higher degree of success, but also have a higher degree of risk.
The physician must work with the patient in assessing all the factors that evaluate both risk and benefit for the patient in their particular circumstance. What is right for one patient may be absolutely wrong for another. This is particularly true for osteonecrosis because each patient presents with a unique set of factors (age, associated disease, specific joint(s) involved, extent and progression of disease). Any treatment needs to be determined between you and your treating physician.
Extent of Disease
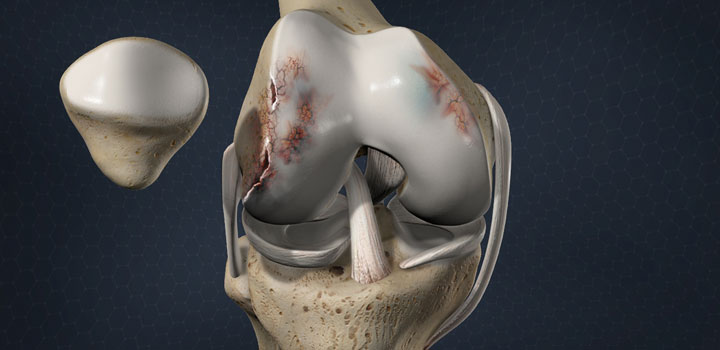
The femoral head is the most frequent bone involved and will be used for this discussion. It is rare for the entire weight-bearing surface of the femoral head to be involved. However, if more than half of the surface is involved, treatments designed to preserve the femoral head have a much lower chance of success.
Progression of the Disease
In the earliest stage of the disease, it cannot be seen by a normal x-ray. Diagnosis is by MRI. Once it can be seen on x-ray, it is not actually the dead bone that can be seen but the response of the living bone to the area of necrosis. The advanced stages begin when the dead bone starts to fail mechanically through a process of microfractures of the bone. Eventually, this will result in damage to the other side of the joint, and need for a total joint replacement.
The greater the extent of the disease and the more advanced the progression, the less likely that the joint can be saved. Fortunately, joint replacement procedures today are highly successful, even in the relatively young patients affected by osteonecrosis. It is always the physicians desire to preserve the normal joint whenever possible. Unfortunately many patients present with advanced, extensive disease.
Non-Surgical Treatment
Protected Weight Bearing
Crutches or a walker are very useful in alleviating the pain associated with osteonecrosis. They can also be useful in protecting the joint between the time of diagnosis and scheduling of elective surgery. They may also play a role in limiting progression while associated medical conditions are managed. However, protected weight bearing alone is never adequate treatment for osteonecrosis and will not result in a cure of the condition, no matter how long it is maintained. Rarely, an associated medical condition may result in a patient not being able to have surgery. In this case, protected weight bearing may be an effective long-term solution for pain control.
Surgical Treatment
Core Decompression
This is a simple surgical procedure, which involves taking a plug of bone out of the involved area. It is applicable for mild to moderate degree of involvement that has not yet progressed to collapse. Because this involves creating a hole in the bone, six weeks of protected weight bearing is necessary to avoid fracture through the hole, one of the complications of the procedure. There is some controversy about this procedure with a few series that have been reported showing generally poor results. However, in centers that do this procedure frequently, most series have reported good results in the appropriate cases.
Bone Grafting
When a section of the bone has died, as is the case in osteonecrosis, for some reason it doesn’t seem to heal. One of the ways that can cause the bone to heal is to surgically remove the dead bone and fill the empty space with bone graft that is either taken from the patient or from the bone bank. The success of this approach depends upon the quantity of bone that has died. Another problem is that during the healing process, which can be very long (6-12 months) the patient must be on weight-bearing restriction.
Vascularized Bone Grafting
Regular bone graft, whether from the bone bank or from the patient is itself dead bone. It serves as a scaffold for the body to build new bone around but the body also has to grow a new blood supply. For this procedure, a bone with its blood vessels is taken from the patient and hooked up to blood vessels near the hip. The dead bone is removed from the femoral head and replaced with the grafted bone that carries with it it’s own blood supply. The advantage of this approach is that the body doesn’t have to rebuild a new blood supply and the bone graft retains its physical and mechanical properties.
Healing and complete filling of the defect still has to take place, during which time crutches or a walker has to be used. The disadvantage also is that a substantial piece of bone has to be taken from the lower leg (the fibula, the smaller bone of the lower leg below the knee). Some patients will develop symptoms in the area from which the bone graft is taken. The operation also takes several hours and requires a team experienced in these techniques.
Osteotomy
Usually it is the main weight-bearing area of the bone that is involved with osteonecrosis. In some cases the bone can be cut below the area of involvement and rotated or turned so that another portion of the bone that is not involved in the osteonecrosis can become the new weight-bearing area. These operations are not very common anymore, but may apply to special cases.
Total Hip Replacement
When the osteonecrosis is advanced to the point that there is involvement of the socket as well, then the only thing that will be effective is either a hip fusion (making the hip completely stiff) or a total hip replacement. Total hip replacement is one of the most successful surgical procedures ever devised. Success rates are usually above 95%! The problem with total hip replacements for patients with osteonecrosis is that it is not uncommon for the patient to have a life expectancy of more than 40 or even 50 years.
With current technology, we don’t think that it is likely that a total hip replacement will last that long. For this reason, many physicians will want to try some procedure to put off total hip replacement for a few years even when it is known that that procedure will not in itself be successful forever. If your disease is advanced, and/or extensive, then total hip replacement may be the only thing that makes sense.